Oncology Program
For decades, the Pediatric Oncology Program has been at the forefront of researching and treating childhood cancers. We're committed to helping our patients access the latest innovations in cancer care, and we're often among the first centers to offer new techniques as they become available. All of our programs are designed specifically for diagnosing and treating children with cancer.
Compassionate medical care is complemented by a wide range of services designed to support the well-being of patients and their families throughout this challenging time. Knowing that undergoing cancer treatment is emotionally difficult, we offer not just a helping hand but a hand to hold.
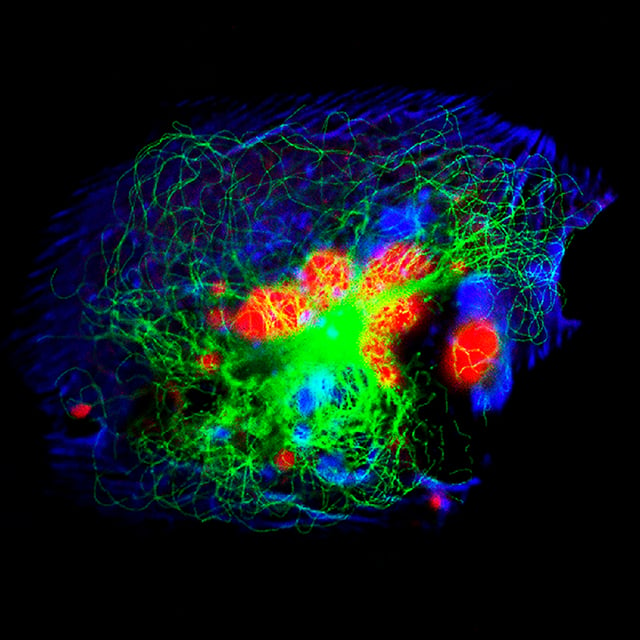
In addition to treating patients, our specialists lead world-class research aimed at advancing the understanding and treatment of cancer in children. Thanks to that work, our patients often have opportunities to participate in large-scale clinical trials of experimental drugs or other promising therapies.
Our overarching goal is to help kids get better as quickly as possible so they can put cancer behind them and get on with their lives. Thanks to the skill and dedication of our team, we're able to make the future brighter for so many of the patients who come to us.
Our locations (3)
Highlights of our cancer care

Leading-edge treatments
We're among the first to offer new treatment options, as soon as they're proven safe and effective. In addition, patients can access promising experimental therapies by participating in one of our many clinical trials.
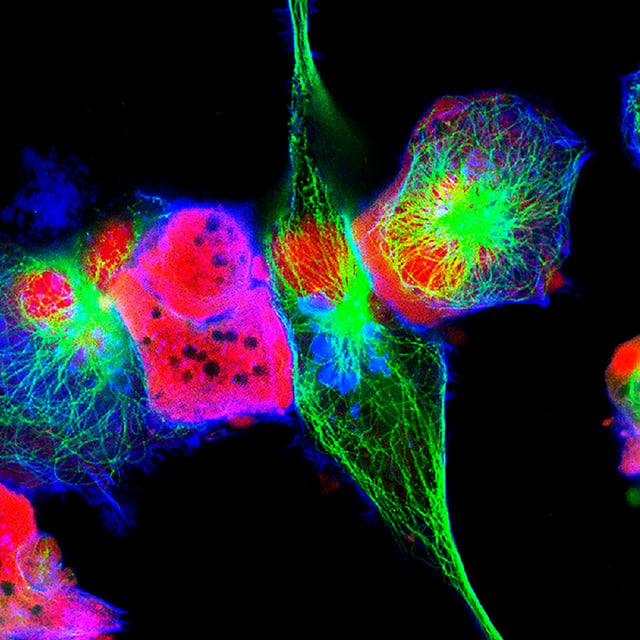
Precision medicine
High-risk tumors are analyzed with the UCSF500 Cancer Gene Panel, a state-of-the-art test that identifies mutations in the tumor's DNA. The results can indicate the best treatment course and, in some cases, clarify the exact type of cancer.
Seamless care, near and far
Dedicated patient navigators help families with managing referrals, insurance concerns and appointment planning. We work with patients and referring doctors well beyond the San Francisco Bay Area, thanks to our comprehensive telehealth system.
Thorough follow-up
Our Pediatric Survivorship Program provides expert care to address any medical, psychological or social issues that arise after treatment is complete. The team also ensures smooth transitions to adult care providers as our patients leave childhood behind.

Our team
-

Anuradha Banerjee
MD
Pediatric Hematology Oncology -

Benjamin S. Braun
MD, PhD
Hematology, Pediatric Medical Oncology -

Maria I. Castellanos
MD
Pediatric Hematology Oncology -

Robert E. Goldsby
MD
Medical Oncology, Pediatric Medical Oncology -

Caroline Hastings
MD
Pediatric Hematology Oncology, Pediatric Neuro-Oncology -

Benjamin J. Huang
MD
Medical Oncology, Pediatric Medical Oncology -

Marie Jaeger-Krause
MD
Pediatric Hematology Oncology, Pediatric Neuro-Oncology -

Rohini Jain
MD
Pediatric Hematology Oncology -

Benjamin Lerman
MD
Pediatric Hematology Oncology -

Anya Levinson
MD
Pediatric Hematology Oncology -

Amanda Marinoff
MD
Pediatric Hematology Oncology -

Jennifer Michlitsch
MD
Pediatric Hematology Oncology -

Sabine Mueller
MD, PhD
Pediatric Neurology, Pediatric Neuro-Oncology -

Brian S. Na
MD, PhD
Neuro-Oncology -

Philip Pauerstein
MD, PhD
Pediatrics, Pediatric Hospital Medicine -

Cheryl Peretz
MD
Pediatric Hematology Oncology -

Bo Qiu
MD, PhD
-

Karen Rabin
MD, PhD
Pediatric Hematology Oncology -

Ruyan Rahnama
MD, PhD
Pediatric Hematology Oncology -

Alyssa Reddy
MD
Pediatric Neurology -

Elizabeth Robbins
MD
Medical Oncology, Pediatric Medical Oncology -

Amit J. Sabnis
MD, MS
Pediatric Medical Oncology, Medical Oncology -

Elizabeth Seashore
MD
Pediatric Medical Oncology -

Elliot Stieglitz
MD
Hematology, Medical Oncology -

Alejandro Sweet-Cordero
MD
Hematology, Medical Oncology -

Russell Valle
MD
Pediatric Hematology Oncology -

Natalie Wu
MD, MS
Pediatric Hematology Oncology -

Elizabeth (Betsy) Young
MD
Pediatric Hematology Oncology -

Kathryn Aaronson
NP
Pediatrics -

Lea Fox
NP, MSN
Pediatric Medical Oncology -

Carly Hoffman
NP, RN
-

Fabienne Hollinger
NP
Pediatric Medical Oncology -

Erin Esaki
PA
-

Anuradha Banerjee
MD
Pediatric Hematology Oncology -

Benjamin S. Braun
MD, PhD
Hematology, Pediatric Medical Oncology -

Maria I. Castellanos
MD
Pediatric Hematology Oncology -

Robert E. Goldsby
MD
Medical Oncology, Pediatric Medical Oncology -

Caroline Hastings
MD
Pediatric Hematology Oncology, Pediatric Neuro-Oncology -

Benjamin J. Huang
MD
Medical Oncology, Pediatric Medical Oncology -

Marie Jaeger-Krause
MD
Pediatric Hematology Oncology, Pediatric Neuro-Oncology -

Rohini Jain
MD
Pediatric Hematology Oncology -

Benjamin Lerman
MD
Pediatric Hematology Oncology -

Anya Levinson
MD
Pediatric Hematology Oncology -

Amanda Marinoff
MD
Pediatric Hematology Oncology -

Jennifer Michlitsch
MD
Pediatric Hematology Oncology -

Sabine Mueller
MD, PhD
Pediatric Neurology, Pediatric Neuro-Oncology -

Brian S. Na
MD, PhD
Neuro-Oncology -

Philip Pauerstein
MD, PhD
Pediatrics, Pediatric Hospital Medicine -

Cheryl Peretz
MD
Pediatric Hematology Oncology -

Bo Qiu
MD, PhD
-

Karen Rabin
MD, PhD
Pediatric Hematology Oncology -

Ruyan Rahnama
MD, PhD
Pediatric Hematology Oncology -

Alyssa Reddy
MD
Pediatric Neurology -

Elizabeth Robbins
MD
Medical Oncology, Pediatric Medical Oncology -

Amit J. Sabnis
MD, MS
Pediatric Medical Oncology, Medical Oncology -

Elizabeth Seashore
MD
Pediatric Medical Oncology -

Elliot Stieglitz
MD
Hematology, Medical Oncology -

Alejandro Sweet-Cordero
MD
Hematology, Medical Oncology -

Russell Valle
MD
Pediatric Hematology Oncology -

Natalie Wu
MD, MS
Pediatric Hematology Oncology -

Shuo Xu
MD
Hematology Oncology -

Elizabeth (Betsy) Young
MD
Pediatric Hematology Oncology
Special programs
Awards & recognition
-

Top 10 in the nation and best in Northern California for cancer care
-

Ranked among the nation's best in 11 specialties
-
Designated an early phase clinical trials core site by the Children's Oncology Group
UCSF's Pediatric Cancer Program

Plan your visit
What to Bring
- Photo I.D.
- Health insurance card
- Insurance authorization, if required
- Doctor's referral, if required
- Recent test results related to your child's condition
- List of medications, including dosages, plus any your child is allergic to
- List of questions you may have
- Device or paper for taking notes
- Completed medical forms that we will mail to you ahead of time
Related clinics (6)
 3
3
Bone Marrow Transplant, Cellular and Gene Therapy Program
 7
7
Hematology Clinic
Support services
Clinical trials
Naxitamab Added to Induction for Newly Diagnosed High-Risk Neuroblastoma
Measured by the presence of radiologically assessable disease by cross-sectional computed tomography (CT) or Magnetic resonance imaging (MRI) imaging and/or by metaiodobenzylguanidine (MIBG) or positron emission tomography (PET) s...
Recruiting
More about this studySilmitasertib (CX-4945) in Combination With Chemotherapy for Relapsed Refractory Solid Tumors
To characterize the safety profile of silmitasertib in combination with chemotherapy
Recruiting
More about this studyPediatric Precision Laboratory Advanced Neuroblastoma Therapy
To measure the response of treatments chosen based on: • Event free survival (EFS)
Recruiting
More about this studyCombination ADI-PEG 20, TMZ, and RT for Treatment of Newly Diagnosed High-grade Glioma (HGG)
Proportion of participants in Phase 1 with treatment-emergent adverse events as graded by National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE version 5.0) will be reported.
Recruiting
More about this studyA Study of Lower Radiotherapy Dose to Treat Children With CNS Germinoma
Will be estimated for eligible and evaluable patients assigned to Stratum 1 using Kaplan-Meier (KM) EFS estimates at 2 and 3 years with respective 80% two-sided confidence intervals. Time from initiation of radiation to the first ...
Recruiting
More about this studyEflornithine (DFMO) and Etoposide for Relapsed/Refractory Neuroblastoma
To evaluate the efficacy of difluoromethylornithine (DFMO) in combination with etoposide in patients with relapsed/refractory neuroblastoma, based upon: o Event free survival (EFS) from time of enrollment.
Recruiting
More about this studyA Study to Evaluate Glofitamab Monotherapy and Glofitamab + Chemoimmunotherapy in Pediatric and...
Recruiting
More about this studyDabrafenib and Trametinib for BRAF V600 Mutant Low-Grade Gliomas
The Rebound rate is defined as increase in tumor size by 25% or more by Response Assessment in Pediatric Neuro-Oncology-Low Grade Glioma (RAPNO-LGG) criteria and/or clinical progression necessitating the re-institution of therapy ...
Recruiting
More about this studyEmbryonal Tumor With Multilayered Rosettes
The median PFS6 is defined as the median number of months for participants in Cohort 1 who have remained progression-free from the date of initial surgical resection until 6 months.
Recruiting
More about this studyOur research initiatives
Tender wagging care
Our therapy dogs spread joy and smiles at the bedside and throughout the hospital.
Visit Child Life services