Staff superheroes
It’s a bird. It’s a plane. It’s a window washer! Dressed as a superhero to clean and brighten your day.


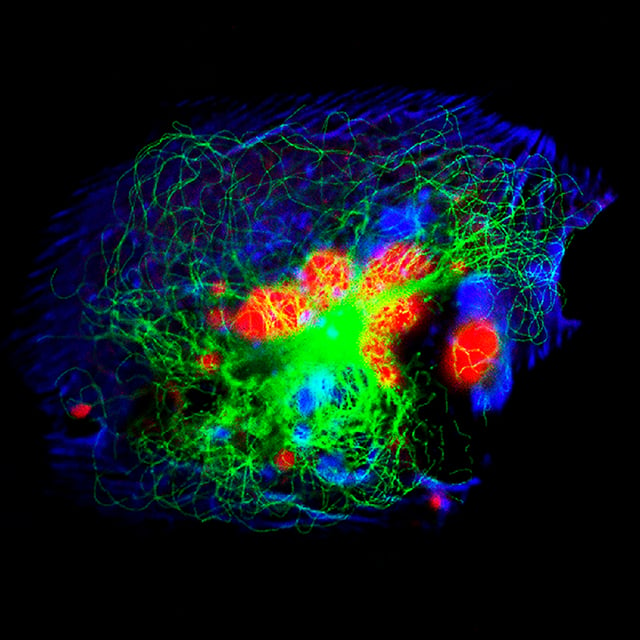
Neuroblastoma is an aggressive cancerous tumor affecting infants and young children. These tumors start in the sympathetic nerve tissues, or the nerves responsible for the body's emergency "fight or flight" response.
The tumor usually begins in the tissues of the adrenal glands, which are in the abdomen on top of the kidneys. These glands secrete hormones and other important substances that are required for normal functions in the body such as the nervous system. The tumor also may begin in nerve tissue next to the spine in the neck, chest or pelvis.
Although neuroblastoma may be present at birth, it often isn't detected until the tumor has grown and compressed surrounding organs. It may also spread to lymph nodes, bones, the central nervous system or bone marrow. In rare cases, pediatric neuroblastoma can be detected before birth by a fetal ultrasound.
In the United States, about 600 children are diagnosed with neuroblastoma each year. It is the most common tumor found in children under 1.

Top 10 in the nation and best in Northern California for cancer care

Ranked among the nation's best in 11 specialties

patients treated with MIBG therapy, a leading-edge neuroblastoma treatment
Neuroblastoma is always linked to a genetic change that causes neuroblastoma cells to divide and grow uncontrollably. In most cases, the gene mutation is spontaneous, occurring for reasons unknown. In a small number of cases, the condition is caused by an inherited gene mutation.
Certain genetic conditions can increase a child’s risk of developing neuroblastoma. These include:
The most common symptoms of neuroblastoma are caused by pressure from the tumor or bone pain from cancer that has spread to the bone and bone marrow.
Symptoms may include:
Other less common symptoms include:
Symptoms also may include:
If your child has symptoms of neuroblastoma, blood and urine tests, tissue samples, and imaging studies will be needed. These diagnostic tests are important because many of the symptoms and signs of neuroblastoma also can be caused by other cancers or by non-cancerous diseases. The tests can confirm if your child has neuroblastoma or another condition.
Your child's nerve cells release chemicals called neurotransmitters that control nerve activity. One type of neurotransmitter called catecholamines, is produced by the sympathetic nervous system. Elevated levels of catecholamines can be found in 90 to 95 percent of patients with neuroblastoma. Blood or urine tests measure these levels.
Your child's doctor may order additional blood tests to check liver and kidney function and salt balance. A urinalysis may be also done to further check kidney function.
Imaging tests produce pictures of the body's interior. Two or more of these tests are generally used to identify tumors in areas where neuroblastomas grow or tend to spread. These tests may include:
Blood and urine tests and imaging studies may indicate that a neuroblastoma is likely present. However, to confirm a diagnosis your child will need a biopsy – a test where the tumor cells are collected and analyzed under a microscope.
If blood or urine levels of catecholamines or their metabolites are higher than normal, then finding cancer cells in a bone marrow biopsy is enough evidence to diagnose neuroblastoma. The disease spreads to bone marrow in about a quarter of patients. Bone marrow can be sampled in two ways, and both are generally done at the same time:
Your doctor may also take tissue samples from the primary tumor. If these samples show certain features of neuroblastoma, the doctor can make a clear diagnosis, even if catecholamine levels are normal. A doctor experienced in testing children's tumor samples can easily recognize neuroblastoma under a microscope.
Sometimes, the features of neuroblastoma can be easily confused with other types of children's cancers, making diagnosis more challenging. In those cases, special tests of the tissue samples are done, including:
When diagnosing neuroblastoma, your child's doctor may describe the cancer using the following categories or terms:
In addition to staging the cancer, the doctors will determine if the cancer is low-, intermediate- or high-risk. Risk is determined by various factors including the stage of the cancer, the child’s age, the aggressiveness of the cancer and how much of the tumor can be surgically removed. The risk level can affect the treatment plan. Low- and intermediate-risk patients have a good chance at being cured. High-risk neuroblastoma is more difficult to cure.
Treatment options will depend on your child's age, the location and biology of the tumor, stage of the disease and the impact on surrounding lymph nodes. More than one method of treatment may be used, depending on your child's condition.
If surgery is an option, it is used to remove as much of the cancer as possible. If the cancer can't be removed, surgery may be limited to a biopsy.
Radiation therapy uses high-energy rays to damage or kill cancer cells and shrink tumors. Radiation usually comes from a machine outside the body, an approach called external beam radiation therapy.
Chemotherapy uses drugs to kill cancer cells and shrink tumors. Chemotherapy drugs may be taken by mouth or injected into a vein or a muscle. Chemotherapy is called a systemic treatment because the drug enters the bloodstream, travels through the body and can kill cancer cells throughout the body.
Chemotherapy may be given after the tumor has been surgically removed to kill any remaining cancer cells. This is called adjuvant chemotherapy. Chemotherapy also can be used to shrink the tumor before surgery. This is called neoadjuvant chemotherapy.
A bone marrow transplant (BMT) is a procedure where healthy bone marrow is used to replace bone marrow destroyed by anti-cancer drugs or radiation. At UCSF Benioff Children's Hospitals, the Bone & Marrow Transplant (BMT) Clinic offers autologous bone marrow stem cell transplants to treat children with high-risk neuroblastoma. This procedure uses high-dose chemotherapy to kill the tumor. Afterwards, the bone marrow is infused with the patient's own healthy bone marrow cells, which were previously removed and stored.
UCSF Benioff Children's Hospitals are one of the few centers in the country to offer MIBG therapy. This treatment is used for high-risk neuroblastomas that have not responded to chemotherapy or that have recurred after treatment. It may be provided alone or in combination with chemotherapy or other medication that make the neuroblastoma cells more sensitive to MIBG. The treatment is only available to patients participating in a clinical trial.
At UCSF, radiation oncologists are pioneering intraoperative radiation therapy (IORT) to treat challenging cases of neuroblastoma. We are one of the few medical centers in the United States that offers this treatment option.
IORT delivers a concentrated beam of radiation directly to neuroblastoma tumors during surgery. This targeted approach means that nearby healthy organs are protected from radiation exposure. Unlike traditional radiation therapy, which requires multiple sessions over weeks, IORT often only requires one treatment.
Advancements in high-dose therapy are improving survival rates for neuroblastoma patients. However, there are still challenges with high-risk tumors.
As described earlier, neuroblastoma is categorized as localized resected, localized unresected, regional, disseminated and special. The treatment plan will vary, depending on the type of neuroblastoma.
Localized resectable neuroblastoma
Your child's treatment may be one of the following:
Localized unresectable neuroblastoma
Initial treatment generally consists of surgery to remove as much of the cancer as possible, followed by chemotherapy. A second surgery may be performed to remove any cancer that remains. Radiation therapy also may be prescribed.
Regional neuroblastoma
Treatment depends on your child's age. If your child is younger than 1, treatment may include the following:
If your child is older than 1, treatment may be one of the following:
Disseminated neuroblastoma
Your child's treatment may be one of the following:
Stage 4S neuroblastoma
Children with this special type of neuroblastoma may not require therapy. You may want to have your child take part in a clinical trial that provides new methods of treatment.
Recurrent neuroblastoma
The selection of treatment for recurrent or progressive neuroblastoma depends on the location and extent of the recurrence and previous therapy as well as individual circumstances. A clinical trial may be appropriate. UCSF Benioff Children's Hospitals participates in national and local studies for recurrent neuroblastoma, including new therapies with targeted radiation (I-131-MIBG), phase I trials of the New Approaches to Neuroblastoma Therapy (NANT) consortium and phase I and II trials of the Children's Oncology Group.
Recurrent or refractory neuroblastoma
Sometimes, neuroblastoma comes back after treatment (recurrent) or doesn't respond to initial treatment (refractory). The treatment options then depend on the location and extent of the cancer, previous therapy as well as individual circumstances.
UCSF Benioff Children's Hospitals medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your child's doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your child's provider.
 3
3
Naxitamab Added to Induction for Newly Diagnosed High-Risk Neuroblastoma
Measured by the presence of radiologically assessable disease by cross-sectional computed tomography (CT) or Magnetic resonance imaging (MRI) imaging and/or by metaiodobenzylguanidine (MIBG) or positron emission tomography (PET) s...
Recruiting
More about this studySilmitasertib (CX-4945) in Combination With Chemotherapy for Relapsed Refractory Solid Tumors
To characterize the safety profile of silmitasertib in combination with chemotherapy
Recruiting
More about this studyPediatric Precision Laboratory Advanced Neuroblastoma Therapy
To measure the response of treatments chosen based on: • Event free survival (EFS)
Recruiting
More about this studyEflornithine (DFMO) and Etoposide for Relapsed/Refractory Neuroblastoma
To evaluate the efficacy of difluoromethylornithine (DFMO) in combination with etoposide in patients with relapsed/refractory neuroblastoma, based upon: o Event free survival (EFS) from time of enrollment.
Recruiting
More about this study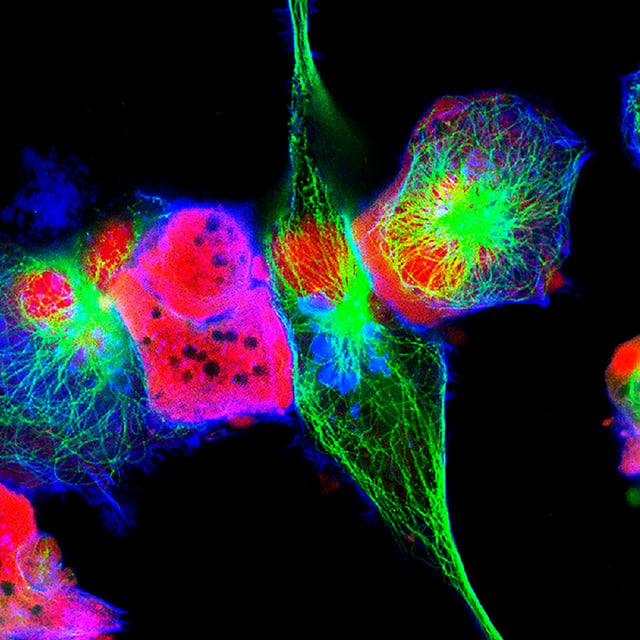
Staff superheroes
