Tender wagging care
Our therapy dogs spread joy and smiles at the bedside and throughout the hospital.
Visit Child Life services

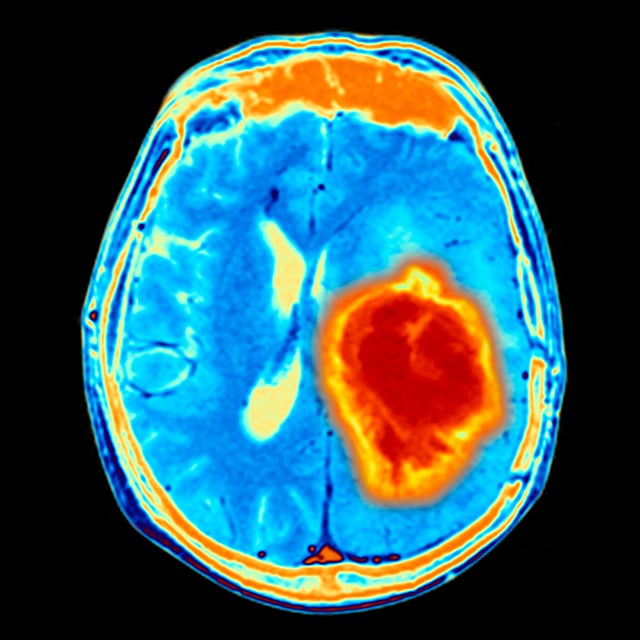
Astrocytoma is one of the most common types of brain tumor that can develop in children. It arises from a specific type of cell in the brain, called an astrocyte. Astrocytomas are divided into subgroups based on their grade and their location in the brain. The grade is determined by what the tumor tissue looks like under the microscope. In general, the lower a tumor's grade, the less aggressive its behavior.
High-grade astrocytomas are either grade 3 or grade 4 brain tumors. Both are malignant, but grade 4 tumors are more aggressive than grade 3 tumors. These tumors most often occur in the cerebral hemispheres but can also occur in the thalamus or, less commonly, in the posterior fossa.
Unfortunately, the outcome for children with malignant brain tumors remains poor. Children with tumors that can be surgically removed tend to have better outcomes than children with residual tumor or tumors that cannot be surgically removed because of their location in the brain.
In most cases we do not understand why children develop high-grade astrocytomas. There is nothing you could have done to prevent this from happening. There are certain genetic syndromes, such as neurofibromatosis, tuberous sclerosis and Li-Fraumeni syndrome, that are associated with malignant astrocytomas, but for most children these tumors occur without identifiable cause.
Most patients with high-grade astrocytomas will seek medical attention because of new seizures, headaches or a neurological problem related to the part of the brain affected. For example, a tumor in the left temporal lobe will often cause speech difficulty as is grows. These symptoms will lead to an imaging study such as an MRI scan that identifies the astrocystoma.
Whenever possible, children with malignant astrocytomas undergo surgery followed by radiation therapy and some form of chemotherapy. Children with high-grade astrocytomas are often treated in clinical trials since no effective treatment has yet been identified.
External beam radiation therapy to the site where the tumor was removed has been shown to improve survival when compared to surgery alone, and is therefore considered the standard of care. The theory is that radiation can kill cancer cells that may be left behind after the surgery.
Although these tumors often grow into the brain tissue, children will do better if all of the tumor that is seen on the scan can be removed. Advanced imaging tools now allow the mapping of important pathways in the brain so that surgery can be performed more safely, reducing the likelihood of causing major neurologic deficits.
For most patients with high-grade astrocytomas, even with aggressive initial treatment, the tumor will return. Once there is evidence of tumor recurrence, there are several options available, including additional surgery, chemotherapy and radiation. The best treatment for a recurrence depends on several factors, such as the tumor's location, time from initial diagnosis and prior treatment. A variety of experimental therapies are also available through clinical trials, and your neuro-oncologist can discuss the different studies with you in detail.
UCSF Benioff Children's Hospitals medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your child's doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your child's provider.

One of the nation's best for neurology & neurosurgery

Ranked among the nation's best in 11 specialties
Tender wagging care
