Fetal surgery firsts
The first open fetal surgery in the world was performed at UCSF in the early 1980s.


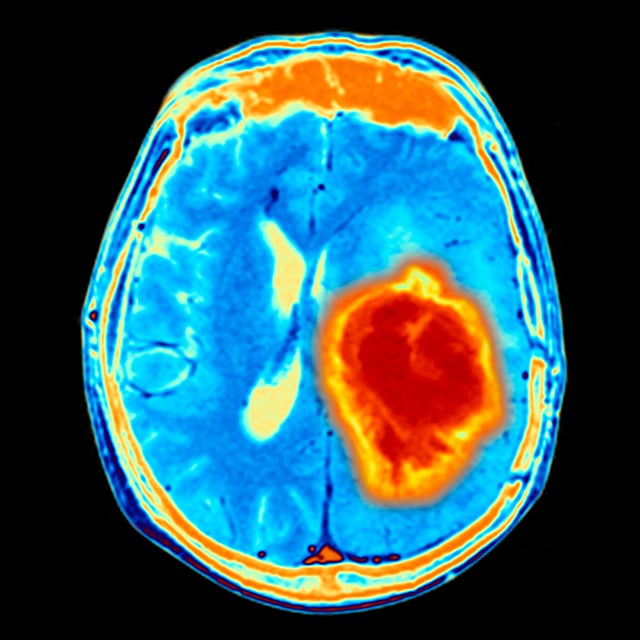
Astrocytoma is one of the most common types of brain tumors that can develop in children. It arises from a specific type of cell in the brain, called an astrocyte. Astrocytomas are divided into subgroups based on their grade and their location in the brain.
A cerebellar astrocytoma is located in the cerebellum, which is the portion of the brain in the lower back of the head. The cerebellum controls balance and other motor functions.
The grade of an astrocytoma is determined by what the tumor tissue looks like under the microscope. In general, the lower the grade of a tumor, the less aggressive its behavior.
Most cerebellar astrocytomas are low-grade tumors (grades I or II) and respond well to treatment. Grade I astrocytomas make up about 80 percent of low-grade cerebellar astrocytomas.
In most cases, we don't understand why children develop low-grade cerebellar astrocytomas. There is nothing you could have done to prevent this from happening. There are certain genetic syndromes, such as neurofibromatosis or tuberous sclerosis, that are associated with astrocytomas, but for the majority of children, these tumors don't have an identifiable cause.
Since the cerebellum controls movements and balance, children with cerebellar tumors often have balance and coordination problems.
The cerebellum is located in a region of the brain known as the posterior fossa. Children with tumors in the posterior fossa also often have increased pressure in the brain that is caused by a build-up of cerebrospinal fluid, called hydrocephalus. Symptoms of increased pressure include headaches, vomiting, increased sleepiness, and vision problems.
The symptoms of low-grade cerebellar astrocytoma usually lead to an imaging study of the brain. Sometimes the initial study is a CT scan, but an MRI scan is usually required to determine the exact location of the tumor and its relationship to other brain structures. Most cerebellar astrocytomas occur on one side in the cerebellar hemisphere. Fluid-filled cysts are common features of these tumors.
The mainstay of treatment for low-grade cerebellar astrocytomas is surgery. During surgery, your child's pediatric neurosurgeon will remove as much of the tumor as possible. Once the tumor is removed, your child will likely be monitored with imaging tests, such as an MRI, to make sure the tumor does not come back. If the tumor cannot be completely removed surgically, or if there is evidence of recurrence, additional treatment is often necessary.
Children with low-grade cerebellar astrocytomas generally have excellent outcomes. Grade I cerebellar astrocytomas have a 10-year progression-free survival of about 80 to 90 percent if the tumor is removed completely with surgery. Grade II astrocytomas are relatively rare in children but carry a worse prognosis. They often recur after surgery, requiring additional treatments such as chemotherapy, radiation or both.
If the tumor recurs, there are multiple options for additional treatment, such as a second surgery, chemotherapy and radiation therapy. Treatment recommendations depend on factors such as the associated risks of another surgery and the child's age.
UCSF Benioff Children's Hospitals medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your child's doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your child's provider.

One of the nation's best for neurology & neurosurgery

Ranked among the nation's best in 11 specialties
Fetal surgery firsts
