Smell the roses
Wander outside into our Butterfly Garden in Oakland and our healing gardens at Mission Bay.


Medulloblastoma is a malignant (cancerous) brain tumor that forms in the cerebellum, the part of the brain that controls balance, coordination and other complex functions. Common symptoms of medulloblastoma include headaches and vomiting. Patients may also have problems with balance and vision when they are diagnosed.
Medulloblastoma is a member of a larger group of tumors called primitive neuroectodermal tumors, or PNETs. All PNETs, including medulloblastoma, have the ability to spread throughout the entire central nervous system.
With aggressive treatment, many patients can be cured of medulloblastoma. However, some forms of medulloblastoma are resistant to treatment, at which point the disease becomes life-threatening. While conventional treatments can be effective for many patients, survivors are at risk for developing long-term side effects. These include:
About 15 to 20 percent of all childhood brain tumors are medulloblastoma. Medulloblastoma is most commonly diagnosed in children and adolescents. For most patients, the cause of their medulloblastoma is unknown. However, there are a few rare, genetic syndromes that may increase a person's chance of developing medulloblastoma, such as:
Because of their location, symptoms caused by the growth of medulloblastomas usually result from blockage of cerebrospinal fluid (CSF) flow or from direct pressure on the brain and cranial nerves. The build-up of CSF in the brain is called hydrocephalus, and causes common symptoms such as:
Direct pressure on cranial nerves adjacent to the tumor can also cause double vision and difficulty speaking or swallowing.
When patients develop frequent headaches with vomiting, or symptoms caused by cranial nerve dysfunction, we usually do an imaging study. Although we often start with a CT scan of the head, an MRI is usually required to provide details of the tumor's location and its relationship to normal brain structures. Typically, we also take additional images of the spine to determine if the tumor has spread to the spinal cord.
Although there are several different kinds of tumors that can form in the cerebellum, it is usually possible to narrow the diagnosis with advanced MRI scans.
The most effective treatment for medulloblastoma is a combination of therapies that include surgery, radiation therapy and chemotherapy. Complete surgical removal of the tumor is important and is usually the first step in treatment. This is usually followed by radiation to the entire brain and spine in older patients (those over 3), followed by several months of chemotherapy.
Standard treatment for very young children — often defined as children under 3 — includes surgical removal of the tumor and chemotherapy. The use of radiation for this age group is controversial, but some doctors are increasingly using radiation restricted to the area of the tumor. Because these young patients cannot tolerate whole brain and spine radiation, intensive doses of chemotherapy are being tested, including high-dose chemotherapy with autologous stem cell rescue, a form of bone marrow transplant.
With aggressive treatment, many medulloblastoma patients can be cured of the cancer. There’s an 80 percent cure rate for patients who are 3 or older and who have average risk disease and are treated with a combination of complete surgical removal of the tumor, radiation and chemotherapy. Average risk disease is defined as compete removal of the tumor and no signs of tumor spread to other parts of the central nervous system and body.
Patients with high-risk disease can still be cured, but the cure rates are lower. Treatment for younger patients, who are more prone to complications from extensive radiation, is evolving. The goal is to identify effective therapies that will hopefully spare the patient the long-term complications of extensive radiation to the brain. With high-risk disease, the tumor has spread or cannot be completely removed with surgery.
UCSF Benioff Children's Hospitals medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your child's doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your child's provider.
Liothyronine in Combination With BIT Regimen for Medulloblastoma With or Without Minimal Residu...
Proportion of participants with adverse events of L-T3 as graded by National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE version 5.0)
Recruiting
More about this studyDFMO as Maintenance Therapy for Molecular High/Very High Risk and Relapsed Medulloblastoma
o To evaluate the efficacy of difluoromethylornithine (DFMO) as a single agent in preventing relapse in patients with molecular high risk and very high risk medulloblastoma, and relapsed/refractory medulloblastoma based upon the 2...
Recruiting
More about this studyIndividualized Treatment Plan in Children and Young Adults With Relapsed Medulloblastoma and Ep...
Time to tissue collection will be used to determine the feasibility of using the results of real-time in vitro drug screening, WES and RNAseq of participant-derived specimens to guide treatment recommendations by a specialized tum...
Recruiting
More about this studyA Study of Treatment for Medulloblastoma Using Sodium Thiosulfate to Reduce Hearing Loss
Will estimate the number and percentage of patients with >= grade 2 hearing loss using the society of pediatric oncology (SIOP) scale (defined as hearing threshold >20 dB at >= 4kHz) 4 weeks after the last dose of cisplatin. If he...
Recruiting
More about this study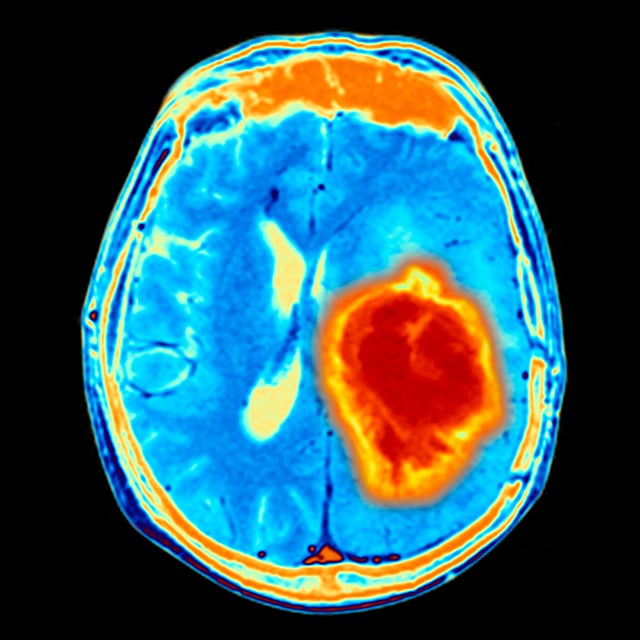

One of the nation's best for neurology & neurosurgery

Ranked among the nation's best in 11 specialties
Smell the roses
