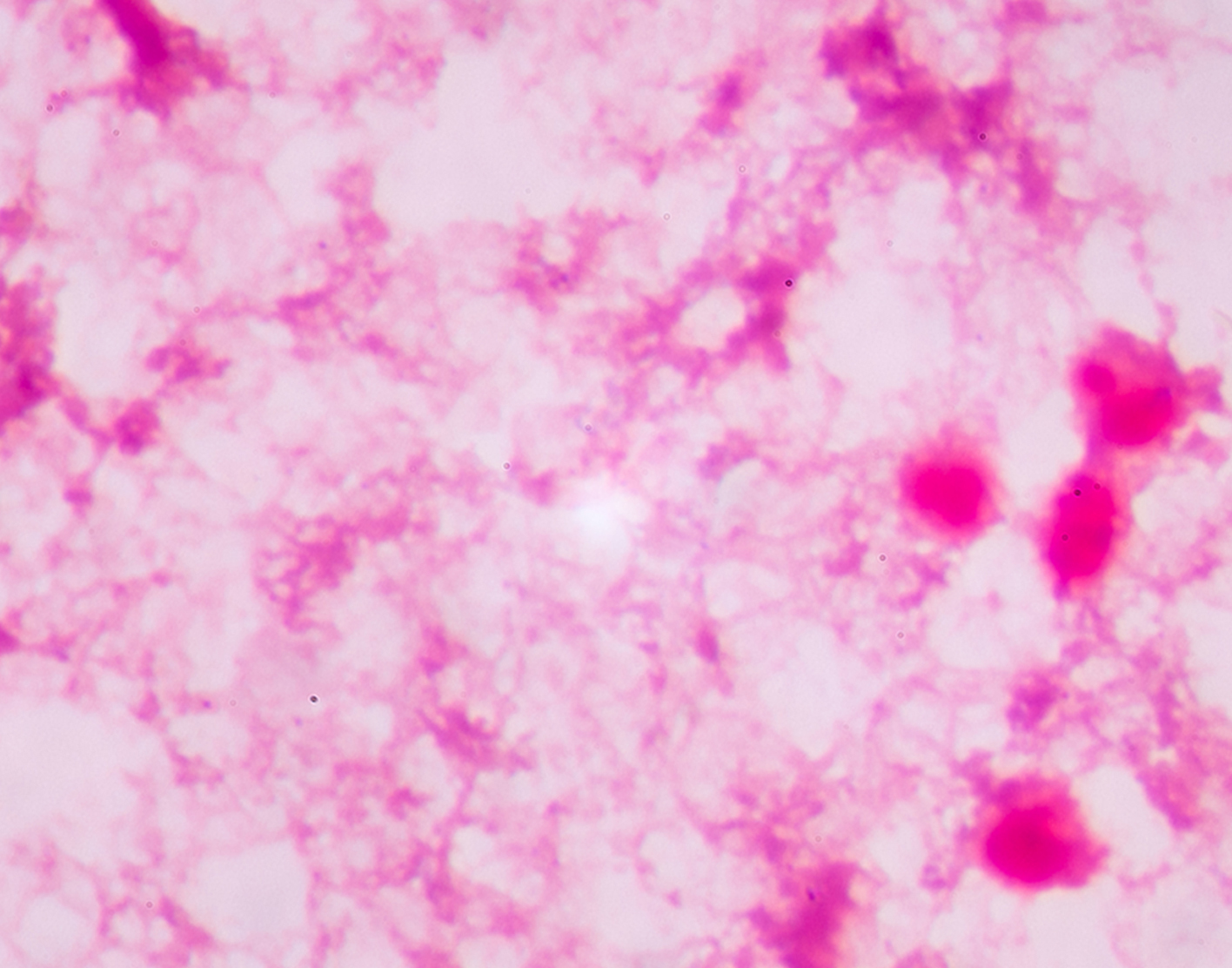
Pleural fluid smear
Definition
Pleural fluid smear is a laboratory test to check for bacteria, fungi, mycobacteria, or abnormal cells in a sample of the fluid that has collected in the pleural space. This is the space between the lining of the outside of the lungs (pleura) and the wall of the chest. When fluid collects in the pleural space, the condition is called
How the Test is Performed
A procedure called
How to Prepare for the Test
No special preparation is needed before the test. A chest x-ray will be performed before and after the test.
DO NOT cough, breathe deeply, or move during the test to avoid injury to the lung.
How the Test will Feel
For thoracentesis, you sit on the edge of a chair or bed with your head and arms resting on a table. The provider cleans the skin around the insertion site. Numbing medicine (anesthetic) is injected into the skin.
A needle is placed through the skin and muscles of the chest wall into the space around the lungs, called the pleural space. As fluid drains into a collection bottle, you may cough a bit. This is because your lung re-expands to fill the space where fluid had been. This sensation lasts for a few hours after the test.
Ultrasound is often used to decide where the needle is inserted and to get a better view of the fluid in your chest.
Why the Test is Performed
The test is performed if you have a pleural effusion and its cause is not known, especially if the provider suspects an infection or cancer.
Normal Results
Normally, no bacteria, fungi, or cancer cells are present in the pleural fluid.
Normal value ranges may vary slightly among different laboratories. Talk to your provider about the meaning of your specific test results.
What Abnormal Results Mean
Positive results may indicate that infection, or cancer cells, are present. Other tests can help identify the specific type of infection or cancer. Sometimes, the test may show abnormalities (such as special types of cells) from conditions such as
Risks
Risks of thoracentesis are:
- Collapse of the lung (
pneumothorax ) - Excessive loss of blood
- Fluid re-accumulation
- Infection
- Pulmonary edema
Respiratory distress
References
Broaddus VC, Light RW. Pleural effusion. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 108.
Ruhl TS, Good JL. Thoracentesis. In: Fowler GC, ed. Pfenninger and Fowler's Procedures for Primary Care. 4th ed. Philadelphia, PA: Elsevier; 2020:chap 218.
Review Date: 06/12/2021
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed physician should be consulted for diagnosis and treatment of any and all medical conditions. Call 911 for all medical emergencies. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. Copyright ©2019 A.D.A.M., Inc., as modified by University of California San Francisco. Any duplication or distribution of the information contained herein is strictly prohibited.
Information developed by A.D.A.M., Inc. regarding tests and test results may not directly correspond with information provided by UCSF Health. Please discuss with your doctor any questions or concerns you may have.